Compare:
Protons, Surgery, X-rays
Cancer is a big business in the United States. More people make a living from it than die from it. It comes as no surprise that medical specialists protect and promote their own turf. Surgeons think surgery is the best. Radiologists think x-rays are the best. Proton therapy centers love proton therapy. And hammers see everything as if it were a nail. My purpose here is to compare proton therapy with surgery and x-rays.
Many of my illustrations will be for prostate cancer, my personal area of experience. The principles, however, apply to most types of cancer. Let me start with two important declarations. First, you are not likely to get an unbiased opinion from a doctor whose specialty is under consideration. Perhaps your family doc will do better, but probably not. Mostly, with proton therapy, you are on your own. Second, I am not a doctor and I am not giving medical advice. If I succeed in my mission to get you curious about proton therapy, please peruse the websites of proton therapy centers (see CHOOSE A CENTER) or contact them directly for a consultation or to ask questions.
ALL TREATMENTS NOT ARE EQUAL
A common myth is that all treatments kill cancer equally well, and therefore, are essentially interchangeable. But what about the treatment itself, the experience, the quality of life, side effects, longevity, recurrence, and many other considerations? At the end of this essay I include an article that I find is more balanced than many. Even so, the author makes this comment (my bolding):
The American Urologic Association periodically reviews all the published series reporting treatment results for prostate cancer and always comes to the same conclusion - Taken as a whole, there is no difference in the likelihood of cure whether one has surgery or radiation therapy. If one method of treatment were clearly superior, it would make life easy. We as physicians would just tell everyone to have that treatment. Since cure rates are equivalent, however, men have to consider their options and decide which treatment they want (or more realistically, which treatment they would least mind having).
This kind of statement concentrates solely on the endpoint, killing the cancer. This is like many drugs, which gain approval by successfully eliminating a specific set of symptoms, but in so doing, create others, some of which can be fatal. Killing cancer is not the only criterion. Patients want the complete picture.
I have a friend who, as a nurse, worked in cancer research decades ago. One modality they tested, microwaves, killed the cancer but caused such devastation and suffering they had to halt their trials. Microwaves would fit under the general statement above as killing cancer, but at what human cost?
While surgery and x-rays do indeed address the cancer, I feel they do not measure up to proton therapy when everything is considered. Therefore, I will discuss each of these modalities. The bottom line: which one would you choose?
Of all the books I read, the best was: An ABC of Prostate Cancer Today by Alan G. Lawrenson. (See: https://www.amazon.com/ABC-Prostate-Cancer-Today-Solutions/dp/1695696395) The author lives in Australia where he works as a medical researcher. When diagnosed with prostate cancer, he had the tools, experience, and knowledge to look into every viable treatment, which he describes in his book. In the end, he chose proton therapy. That got my attention.
Lawrenson’s insurance did not cover proton therapy. So, he traveled to South Korea to receive it at a cost of tens of thousands of dollars at his own expense. He did this even though his insurance would have covered the other treatments and cost him nothing. Clearly he thinks highly of proton therapy. So do patients surveyed as to their experience, as indicated in the chart below.
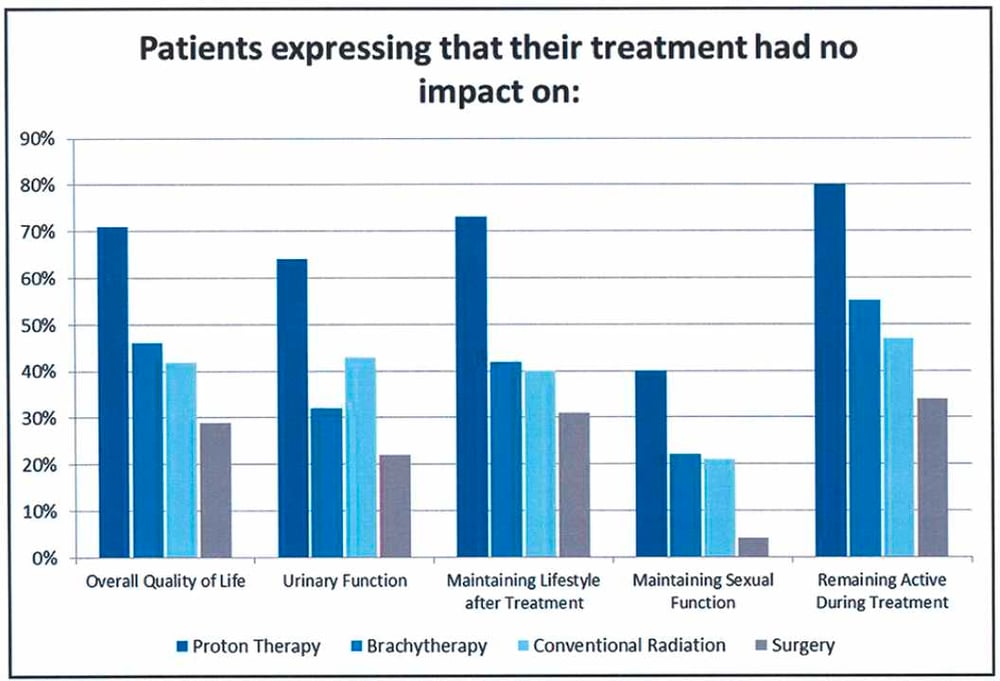
In the above survey, proton therapy really shines, having the highest bars of approval in each category (on the left). Not theoretical, not manipulated statistics, the graph reflects the response from real people who underwent those modalities and how they rate them.
SURGERY - NOT THE GOLD STANDARD
Surgery claims to be the gold standard. For example, on one website I found the following statement: “Surgery to remove the prostate gland, sometimes with some surrounding lymph nodes is one of the surest ways to treat localized prostate cancer.” There’s only one problem. That isn’t true.
The New England Journal of Medicine published a ten-year study of 1,643 men with prostate cancer (September 14, 2016, DOI: 10.1056/NEJMoa1606221.) The study, which divided participants between watchful waiting, surgery, or radiation (x-rays), reached these conclusions.
Of the three treatments, prostatectomy had the greatest negative effect on sexual function and urinary continence, and although there was some recovery, these outcomes remained worse in the prostatectomy group than in the other groups throughout the trial.
“Throughout the trial” means surgery had the worst effects for ten years. Some gold standard. My proton therapy treatment resulted in no side effects, no pain, no change in quality of life. Some people call it a radiation vacation (see EXPERIENCE), a huge contrast with the following description of surgery.
You stay in the hospital overnight. You go home with a catheter that stays in for a week. You will have a little bag to catch the urine, and a larger one to use at night. Then, you will wear pads. After two months, you are likely to be pretty well. Maybe a little leakage here and there. After a year, you should be back to normal. Surgery removes one sphincter muscle with the prostate, but you have another one. Doing Kegel exercises should strengthen the remaining one. Maybe, if you do something very energetic, you might leak a little from time to time.
The video the surgeon showed about robotic surgery scared me even more than the above description. The urethra is a tube that transports urine from the bladder out through the penis. It goes right through the prostate. When you remove the prostate, you must then reattach the severed ends of the urethra. This involves having a catheter while the connection heals. It also shortens the penis by an inch or more. Frankly, I didn’t feel like I had a lot to spare, but I suppose that wouldn’t matter, since erections would be a thing of the past, replaced, perhaps, by diapers.
Online (see: https://urologyweb.com/robotic-prostate-surgery-complications/) I found a critical review of robotic surgery by Dr. Bert Vorstman MD, MS, FAAP, FRACS, FACS. (A have no idea what those credentials mean.) The following paragraphs come from Dr. Vorstman.
Robotic prostate cancer surgery not only fails to save significant numbers of lives, it is associated with more complications than probably any other type of cancer surgery.
This toxic, so-called treatment has never been proven to be safe or effective through any scientifically conducted, evidence-based studies. It simply took on a life of its own because medical device manufacturers and urologists were never held accountable.
Not only does prostate cancer surgery fail to save significant numbers of lives but, the complications associated with this reckless “treatment” are common, severe and often, last lifelong. A partial list of complications includes death, hemorrhaging, embolism, bowel, bladder, ureteral and nerve injuries, infections, hernias, positioning pressure injuries to muscles and eyes, foreign bodies, depression and, suicide.
This lack of proof is ironic, as critics of proton therapy, who embrace robotic surgery, demand unreasonably high scientific proof of proton’s efficacy. X-rays also escaped the proof now demanded for proton therapy.
Every man facing prostate cancer should know about the organization called the Brotherhood of the Balloon, or BOB. It is a group of prostate cancer patients who have chosen proton beam radiation therapy. The organization was formed in December 2000 by Bob Marckini and several other patients treated in Loma Linda, California, at the first proton therapy center. Today they have nearly 10,000 members from all 50 states and 39 different countries. Their newsletters are entertaining and informative. (see: www.protonbob.com).
More to my point is the best-selling book written by Robert Marckini, now in a new edition, called You Can Beat Prostate Cancer, And You Don’t Need Surgery To Do It.
Shockingly, according to Dr. Mark Scholz, an oncologist specializing exclusively in prostate cancer, 80% of the operations could have been avoided. “Four out of five operations to remove all or part of the prostate gland are unnecessary,” Scholz told Newsmax.TV.
Dr. Scholz has a very high opinion of his x-ray technologies. Of course, he doesn’t have protons, so he has no other choice. He has many videos on YouTube and damns proton therapy by faint praise, with statements such as, “Well, it does as well as x-rays so if you don’t mind the needlessly high cost, it will certainly give you a good result.” (That’s not a direct quotation, just my attempt to reproduce his casual down putting.) So, although I’m not a fan of Dr. Scholz, neither is he a fan of surgery.
In her article "Regrets After Prostate Surgery" for the New York Times, Tara Parker-Pope wrote:
One in five men who undergoes prostate surgery to treat cancer later regrets the decision, a new study shows. And surprisingly, regret is highest among men who opt for robotic prostatectomy, a minimally invasive surgery that is growing in popularity as a treatment.
The research, published in the medical journal European Urology, is the latest to suggest that technological advances in prostate surgery haven’t necessarily translated to better results for the men on which it is performed. It also adds to growing concerns that men are being misled about the real risks and benefits of robotic surgical procedures used to treat prostate cancer. (see: https://archive.nytimes.com/well.blogs.nytimes.com/2008/08/27/regrets-after-prostate-surgery/)
Curative treatment is only beneficial to younger men who are likely to survive prostate progression. Because of treatment side-effects, older men with shorter life expectancy rarely benefit from radical treatments such as surgery.
Most notably, surgery impairs sexual function, with more than 50% of treated men developing long-term erectile dysfunction. Surgeons try to prevent this by using nerve-sparing techniques, when possible, to reduce the damage to the nerves that control erection. The surgeon peels back the nerves surrounding the prostate prior to removing it. This poses a danger of microscopic prostate cancer clinging to those nerves, later developing into cancer recurrence.
Incontinence also results from many prostate surgeries. Let’s be clear, some of these side effects occur with proton therapy as well. But rarely to the same extent. The Seattle Cancer Care Alliance offers this article about proton therapy vs surgery: https://www.sccaprotontherapy.com/newsletter/june-2018/sci-med-jun-18
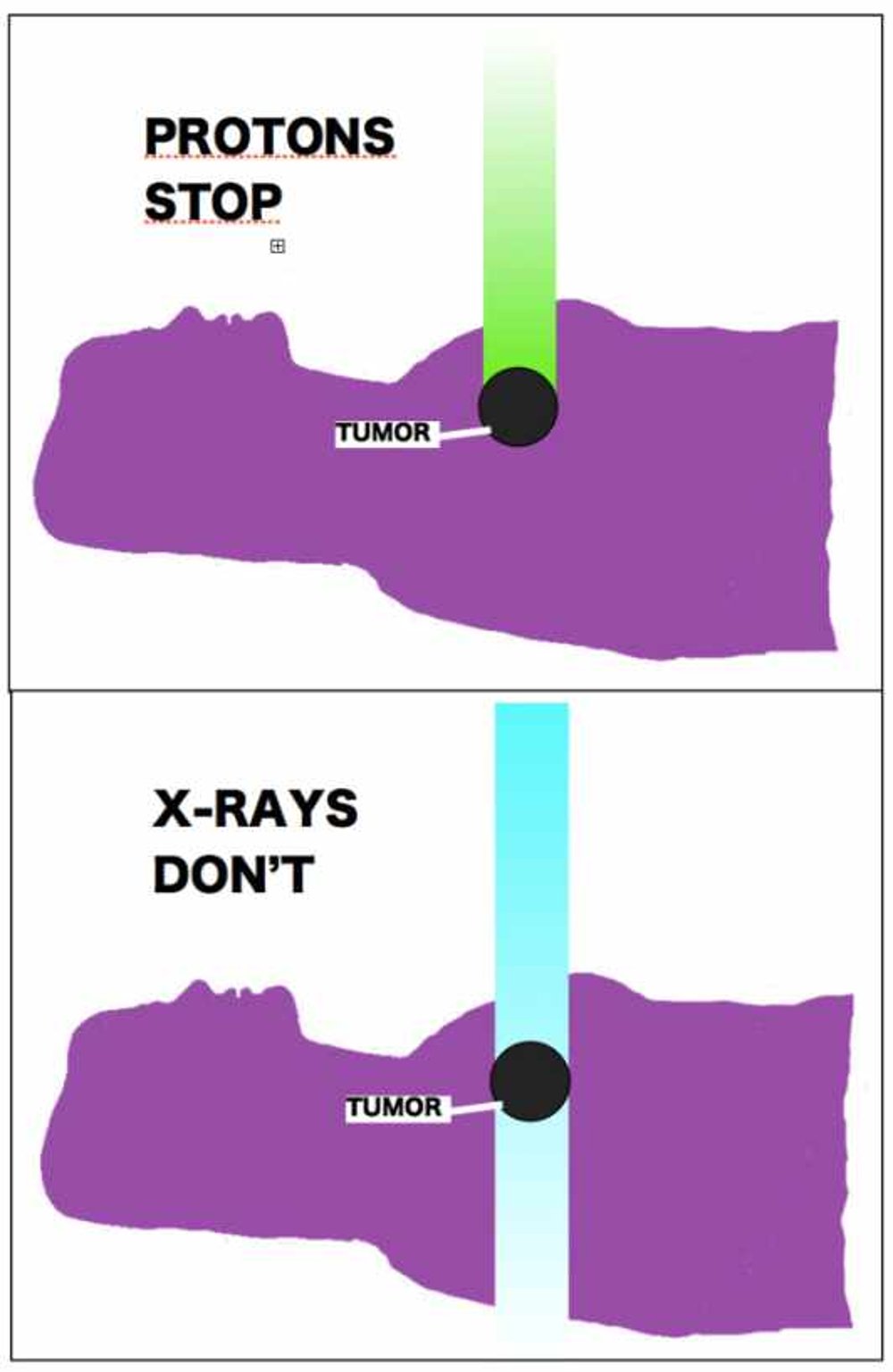
X-RAYS WILL NEVER STOP
No matter how you manipulate x-rays, from whatever multiplicity of angles and numbers of rays, they can never stop. This advantage will always rest with proton therapy. (See: PHYSICS)
Early on, critics questioned whether protons could be as effective as x-rays. Now, radiologists scramble to show that x-rays are as effective as protons, or have as few side effects.
Most casual descriptions of proton therapy point out that it is a type of radiation, like x-rays, but composed of charged protons. They miss the most important characteristic of protons, that they have mass. Protons are wrecking balls whereas x-rays are baseballs. Besides ionizing cancer cells (stealing their electrons, disabling them), protons physically damage the DNA strands of the cancer, creating double-strand breaks whereas x-rays cause mostly single strand-breaks.
The internet contains some pretty outrageous claims from radiologists. Here is an egregious example from a radiologist who uses CyberKnife. First, a few words about CyberKnife. It is a brand name for an x-ray technology called stereotactic body radiation therapy (SBRT). It is a lightweight linear accelerator mounted on a robotic arm. Near real-time images allow for patient movement tracking with considerable accuracy.
This is as good as x-rays get. The machine is robotic, uses artificial intelligence, and is very impressive. It requires a relatively small number of sessions. They like to refer to the procedure as radiosurgery, but that is a bit of a misnomer (dramatic branding) as there is no knife, and nothing gets physically cut out. They are still using x-rays, and they still engulf the body in radiation. Here is a rather engaging (if not somewhat terrifying) YouTube video of CyberKnife session for prostate cancer: https://www.youtube.com/watch?v=keWb1mVh_4I
Now, a quotation and a chart supposedly comparing CyberKnife and proton therapy.
Both CyberKnife and Proton are forms of radiation, however CyberKnife has many advantages over proton beam radiation as a prostate cancer treatment. CyberKnife is the most advanced treatment available, using image-guided robotics to destroy tumors while preserving the surrounding tissue.
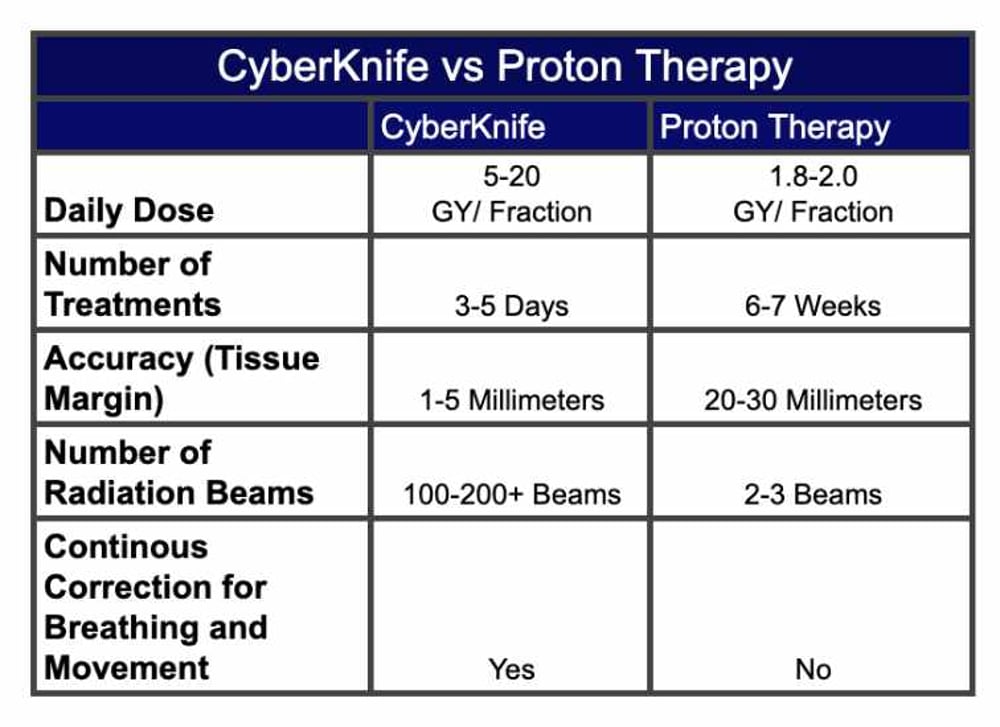
This comparison is completely bogus. Proton therapy also has protocols with as few as five sessions (called hypofractionation). The tissue margin for pencil beam scanning can be millimeters. The claim above, of 20-30 millimeters, computes to over an inch. Really? Protons miss the target by an inch? Get real. Yet the website on which I found this false comparison looks professional, sounds reasonable, and comes across as very professional. And totally wrong. Misinformation at its worst.
I have nothing bad to say about CyberKnife itself, which uses as up to 200 separate rays. I found a study that concluded patients with liver cancer had longer survival with proton therapy, even though those patients were older and not in as good of health as those treated with SBRT. Here is the link to that article.
https://pubmed.ncbi.nlm.nih.gov/31602338/
I worry about all the tissue exposed to radiation, even lower doses. Those 200 x-rays (at higher intensity than protons) still enter the body at higher doses and still exit out the other side of the body. What about secondary cancer down the road, caused by the treatment?
Nancy P. Mendenhall, MD reports in The International Journal of Radiation, Biology, Physics (Vol. 88, Issue 3, pp. 596-602) that intensity modulated radiotherapy IMRT (a type of x-ray) increases the risk of potential recurrence for prostate cancer by fifteen times! MD Anderson Clinic in Houston calculated for esophageal cancer, x-rays have a whopping 96% additional cancer risk. How can CyberKnife overcome that?
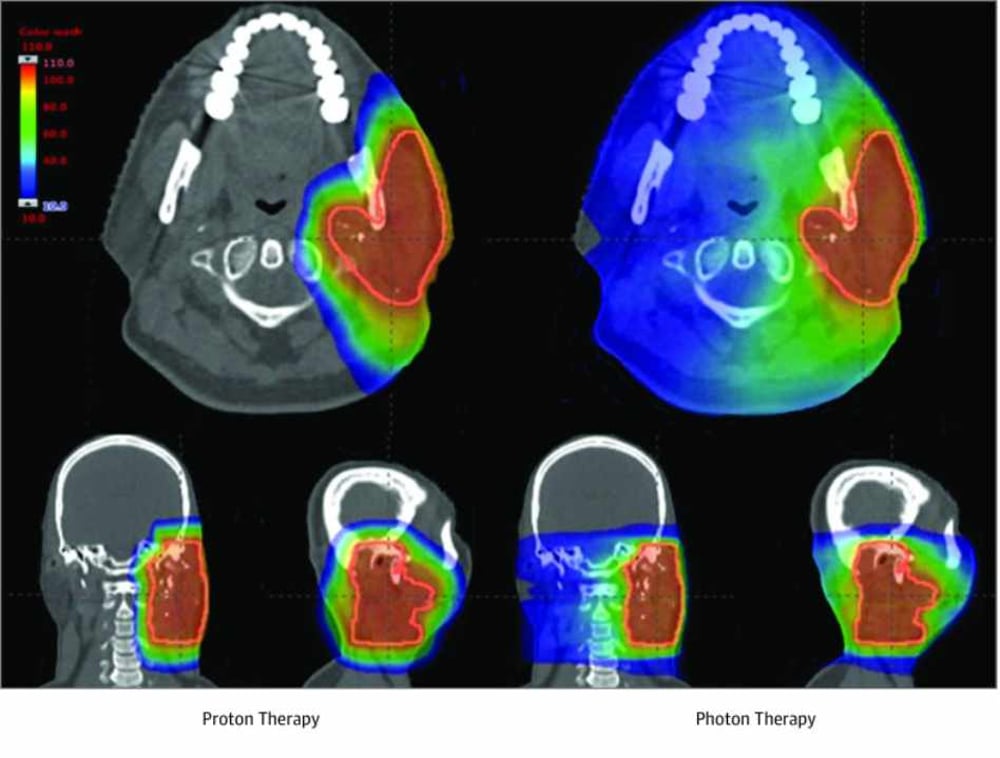
Below is an illustration for head and neck cancer, comparing proton therapy on the left with multiple x-rays on the right. Certainly all of that excess radiation can’t be good for you.
I consider it futile to engage in battling statistics and trials. For example, I can cite a study in which protons combined with chemotherapy did vastly better than x-rays and chemotherapy. Published in the prestigious Journal of the American Medical Association (JAMA), the study included different cancers (not prostate). Their conclusion:
In this comparative effectiveness study of 1483 adults with nonmetastatic cancer and treated with curative intent, proton therapy was associated with a two-thirds reduction in adverse events associated with unplanned hospitalizations, with no difference in disease-free or overall survival.
Here is the link to the article: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6990870/
I can give hundreds of examples like this, in which protons prove to be superior. In a different essay, I give a startling example of how studies can be manipulated, yielding unrepresentative results (see ISSUES).
The critics of proton therapy say they want more direct comparisons between protons and photons. Yet their own technologies have had very few. In fact, that seems especially true with treatments for prostate cancer. In 2017 the New York Times had an article about SMRT titled “Popular Prostate Cancer Therapy Is Short, Intense and Unproven” (see: https://www.nytimes.com/2017/03/20/health/prostate-cancer-sbrt-radiation-therapy.html)
Randomized double-blind studies involve hundreds of people and cost many millions of dollars. A prime example currently underway is the COMPPARE trial (note, two Ps, not a typo). Participants include some fifty clinical sites. The effort is very impressive, and the results beyond criticism. Take a look at their website: https://comppare.org/
RETURN TO PROTON PAGE
GO TO HOME PAGE
Wow, are you still with me? As your reward I have included a relatively balanced discussion of cancer modalities. (See the original here: https://www.medicaldaily.com/prostate-cancer-treatment-vs-removal-surgery-side-effects-and-prognosis-each-404675)
Prostate Cancer Treatment Vs. Removal Surgery: Side Effects And Prognosis Of Each
As far as curing the cancer, there are several options with an equally good probability of doing this, so each patient's decision comes down to "Which set of side effects would I least mind going through?"
The American Urologic Association periodically reviews all the published series reporting treatment results for prostate cancer and always comes to the same conclusion - Taken as a whole, there is no difference in the likelihood of cure whether one has surgery or radiation therapy. If one method of treatment were clearly superior, it would make life easy. We as physicians would just tell everyone to have that treatment. Since cure rates are equivalent, however, men have to consider their options and decide which treatment they want (or more realistically, which treatment they would least mind having).
Before going any further, there are a few things to keep in mind.
Not everyone with prostate cancer needs to be treated - active surveillance is appropriate for many men - at least for a short time and perhaps for a lifetime.
There are only two methods of curing prostate cancer - surgery and radiation therapy. Things like cryotherapy, High Intensity Focused Ultrasound, microwave heating, laser ablation and a few other methods may be appropriate for prostate cancer that recurs after primary treatment, but these are not curative by themselves.
Androgen suppression (hormone therapy) will stop the progression of most prostate cancers, make the PSA drop to (essentially) zero and make masses or bone metastasis shrink away - but its effect is only temporary - lasting a few months to a few years. Like the methods listed above, is not a curative treatment by itself (although it may be combined with radiation therapy to increase its likelihood of cure). Androgen suppression has its own set of side effects including fatigue, loss of muscle mass, weight gain, loss of libido, impotence, osteoporosis and depression.
Urologists are fond of telling patients that "If you have surgery, you can always have radiation afterward, but if you have radiation, you can't have surgery afterward" which is, for the most part, a true statement, but this generalization omits some important facts.
First, It is rarely necessary to have surgery on one's prostate after radiation therapy, since most men who are not cured of their disease don't have recurrence in their prostate gland. Instead, most men who are not ultimately cured of their cancer had subclinical disease beyond the prostate that could not be detected prior to starting treatment. It just takes some time for these undetectable deposits of cancer cells to grow enough so that they eventually cause an elevation of the PSA, independent of any PSA being produced in the prostate.
If someone does have a persistently elevated PSA following treatment with radiation therapy - and if repeat biopsies of their gland are positive (oh, and by the way, post-irradiation biopsies are only reliable starting about two years after the completion of radiation therapy, since it takes time for cancer cells to die after being treated), then there is only a 50:50 chance that their recurrence is only in the gland.
Salvage prostatectomy can be performed after radiation therapy, although it is a difficult operation due to the intense fibrosis around the gland and the decreased blood supply - both of which are as a result of the prior radiation therapy. These operations are best performed at a major urologic center where they do quite a few of them, as opposed to being done by a community urologist. Even in the best of hands, there is a high risk of incontinence following a prostatectomy performed after radiation therapy.
Since there is only a fifty/fifty chance that the recurrent cancer is only in the prostate, there is only a fifty/fifty chance that the surgery will result in a cure.
Not only can you have radiation therapy after surgery, but 20 to 30 percent of the time, you must have radiation after surgery (since that is how often the pathologist finds cancer that has been cut through at the edge of the specimen) in order to be cured. Post-operative radiation therapy results in a ninety percent chance of sterilizing any residual cancer found by the pathologist. And, by the way, when surgeons report their overall cure rates, they include the patients that were only cured due to having post-op radiation therapy (although they seldom mention this in their publications).
Prostate cancer is generally slow growing.
Don't let anyone rush you into making a decision that will have consequences for the rest of your life.
The term "Early Stage" prostate cancer refers to the fact that it is still localized to the prostate or at least in the immediate peri-prostatic tissue. Early stage cancer can still be low, intermediate of high risk based on its Gleason score (assigned by the pathologist after examining the biopsy material), the PSA level and to some extent, the number of positive biopsy cores.
There are basically two methods of performing a prostatectomy:
Open - where the surgeon makes an incision from just above the pubic bone to the belly button and dissects out the prostate (and some lymph nodes), then connects the neck of the bladder to the remaining urethra (since the intervening prostatic urethra is no longer there), and leaves a catheter in place for a few weeks to allow everything to heal back together.
Robotic - which is basically the same operation, but is performed through small incisions using remotely controlled robotic arms and stereoscopic visualization. Dissection is more precise (in experienced hands) and in-hospital stays are shorter. Publications report the potential for a reduced incidence of side effects like infection and bleeding, but it's difficult to tell if the major long term complications like impotence and incontinence are any less.
The major side effect that surgery has that radiation therapy doesn't is incontinence. Most men require one to two months to regain continence after surgery and overall, about five percent never regain urine control (wearing a diaper the rest of their lives).
Impotence is more common with surgery than with radiation therapy. Although surgical series frequently report potency preservation rates above 50 percent, they define potency as the "ability to obtain an erection sufficient for vaginal penetration". So if you can have sex for 30 seconds, you are counted as being potent by the urologists.
I had surveyed the first 150 men on whom I had performed brachytherapy (back in the mid-nineties) and and simply asked the question "Are you satisfied with your sex life?" and left room on the survey form for them to elaborate. Over 60 percent said that they were satisfied with their function (and no one who said they could only achieve penetration said that they were).
At our Proton Center, we survey every man we have treated with two Quality of Life measurement tools on each follow-up visit. One is the "Expanded Prostate Cancer Index Composite" or EPIC questionnaire and the other is the SHIM (Sexual Health Inventory for Men). We have over 2,600 patients in our database so far and over 70 percent have scores indicating satisfaction with their function.
So - overall, men do vastly better with sexual function and infinitely better with continence (since we end up dividing essentially by zero - incontinence almost never occurs with radiation therapy) if they are treated with radiation therapy as opposed to surgery.
So what's the down side of radiation therapy? I'll address these as they relate to each of the various ways in which radiation therapy may be given.
For patients with low risk, localized disease (Gleason 6 histology with a PSA less than 10 and fewer than 4 positive biopsy cores), brachytherapy can be used as monotherapy. Patients come for a mapping procedure where the exact contour of the prostate is outlined every 5 mm from top to bottom using trans-rectal ultrasound and then a three dimensional reconstruction is created in the computer treatment planning system. An optimal arrangement of radioactive seeds is calculated and pre-loaded into needles for placement in the gland. The day of the procedure, the patient is placed under general anesthesia and 20 to 40 needles are used to place 60 to 120 seeds in the prostate under trans-rectal ultrasound guidance.
The patient usually goes home in a few hours and may have a catheter over night (since the gland may swell somewhat and it's better to have the catheter already in place, than to come to the ER in the middle of the night when you can't pee). Men usually have pretty severe irritative voiding symptoms (frequency, urgency, nocturia, decreased stream force) for the next month which resolve over the following month.
They may have some irritative rectal symptoms for a few weeks and can develop a rectal ulcer one to two years after the procedure if some of the seeds end up being right next to the rectal wall. This rectal ulcer always heals up with time as long as a gastroenterologist doesn't biopsy it (thinking it is suspicious for cancer), in which case it may never heal and the patient ends up needing a colostomy.
If someone has risk factors beyond those described above, then brachytherapy alone (brachytherapy as monotherapy) does not result in a sufficiently high cure rate (due to the involvement of periprostatic tissues beyond where the seed irradiation can reach) and must be supplemented by twenty-five external beam radiation therapy treatments (to increase the dose to the periprostatic tissues).
Since the main advantage of brachytherapy is to shorten the length of time it takes to get the treatment, once you add five weeks to get the external beam component, much of that advantage is lost. In the case of higher risk disease, the brachytherapy basically replaces the final nineteen external treatments one would have if they had external beam radiation therapy definitively (which usually consists of 44 treatments over nine weeks).
So if someone has intermediate to high risk disease, they would probably opt for definitive external beam radiation therapy as opposed to going through the procedure for brachytherapy in addition to twenty-five of the external treatments.
So what is the procedure for, and what are the side effects of, definitive external beam radiation therapy for prostate cancer. External beam treatment can be given with high energy x-rays (using a technique knows as Intensity Modulated Radiation Therapy or IMRT) or with Proton Therapy and I'll discuss the differences in these two modalities momentarily. By the way, the Cyberknife, tomotherapy and a variety of linear accelerators deliver IMRT treatment with x-rays - there is no difference in the end result, just the machines being used to deliver it. You may also hear the term IGRT which stands for Image Guided Radiation Therapy, which simply means that some sort of imaging (CT, portal imaging, stereoscopic x-rays, etc.) are performed with the patient on the treatment table just before the treatment is delivered. IGRT is used with all forms of IMRT as well as with Proton Beam Treatment.
For either method of treatment (Protons or x-rays) treatment planning begins with a thin slice CT scan which is fused with a highly detailed MRI. The CT is necessary to tell the treatment planning computer what the tissue density is at all points through which the radiation beams will pass. The MRI gives better anatomic detail for contouring the prostate, seminal vesicles, bladder, rectum, etc.
After several days of contouring structures and running multiple trials of beam arrangements, beam modulation, etc., an optimal treatment plan is developed. Then, the physicists run quality assurance tests to verify that the computer predictions achieve the planned dose distribution in tissue. Finally, the patient returns for the initial "Image Guidance" and the first of 44 treatments.
The radiation oncologist sees each patient weekly and manages any side effects they may have. For x-ray (IMRT) treatments side effects may include fatigue, sometimes to the point that they need to go home and take a two hour nap in the afternoon.
A few weeks into treatment, rectal irritation may begin which can range from mild diarrhea to pain, bleeding and a continual feeling of needing to have a bowel movement, even though there may be nothing besides a little mucous in the stool.
Also, a few weeks into treatment, urinary irritative symptoms such as frequency, urgency, slow bladder emptying, and nocturia (getting up several times at night to urinate) may begin and last until a few weeks after the treatment is over.
Long term risks include the development of radiation induced cancers.
Other than the long term risk of developing a secondary cancer, most side effects resolve within a few months to a year after the radiation therapy is over.
For Proton Treatment
Fatigue is minimal or non-existent. (I treated an avid cyclist a few years back who rode his bicycle over a thousand miles during the nine weeks he was receiving treatment).
Rectal symptoms are almost unheard of (since such a small volume of the rectum is receiving radiation - basically just the part immediately adjacent to the prostate). Urinary irritative symptoms may occur over the same time course as they do with x-ray treatment, although they are generally less severe than with x-rays.
Multiple epidemiologic studies have shown that there is only a minimal increase in the risk of radiation induced cancers with protons as opposed to x-rays - likely due to the much smaller volume of tissue receiving any radiation dose. The few side effects men do have, usually resolve within a few weeks after proton irradiation is over.
What about the data on the relative side effects of Proton Therapy vs. IMRT?
We pooled our data with various cancer centers in order to study about 1,000 patients who had been treated for prostate cancer with Proton Beam Therapy and compared their Quality of Life scores (in the domains of urinary and bowel function) with those of a control group of men who had no treatment (because they didn't have prostate cancer).
The EPIC questionnaire was completed by all men every three months from the beginning of treatment until at least one year after treatment. The results showed that men who were treated with proton therapy for prostate cancer had the same urinary and rectal quality of life scores as men who didn't even have prostate cancer.
Don't let anyone rush you into making a decision that will have consequences for the rest of your life.
RETURN TO PROTON PAGE
GO TO HOME PAGE